Twenty fetal monitoring myths that won’t go away

Myths about fetal heart rate monitoring are plentiful. Here are twenty of them. Let me know if there are others you would like to see me tackle!

Myths about fetal heart rate monitoring are plentiful. Here are twenty of them. Let me know if there are others you would like to see me tackle!

A recent Australian study investigated women’s experiences with various fetal monitoring methods during labor, finding that wired CTG was predominant. First-time mothers reported more CTG use, which correlated with higher emergency cesarean rates and epidural use. Many women felt monitoring negatively impacted their experiences, highlighting a need for improved woman-centered maternity care practices.
The article reviews a recent paper on fetal monitoring during labor by Richmond et al. which lacks a reference list, undermining its educational value. While it identifies some correct points about fetal heart rate interpretations, it perpetuates outdated practices and fails to acknowledge the need for consent in monitoring, thus serving more as promotional content than genuine education.
A recent study examined intermittent auscultation during labor in various UK birth settings. It found that local policies exist in most units, but training and competency assessments were inconsistently implemented. The reliance on certain fetal monitoring devices and practices raises concerns, as does the use of outdated training programs and practices.

Maternity professionals face pressure to continuously record fetal heartbeats, leading to interventions that prioritise monitoring over women’s birth priorities. Evidence suggests that uninterrupted heart rate tracing does not improve neonatal outcomes and can increase complications. The focus should be on overall fetal wellbeing rather than solely on heart rate data accuracy.

The design of the very first RCT about CTG monitoring is interesting, and it raised a question which we really haven’t ever answered fully. Does the use of CTGs create the very problem they are meant to prevent?
Women planning a vaginal birth after cesarean (VBAC) often seek to avoid negative experiences with CTG monitoring. This new mini-course offers reliable information on fetal monitoring options during VBAC, cutting risks down to realistic size, and providing communication strategies with care providers.
Today’s post reflects on a 1959 trial concerning “fetal distress”. It highlights findings that meconium was a critical indicator of poor outcomes, while abnormal fetal heart rates weren’t reliably predictive. Should we be reevaluating current obsessions with CTG use and focusing on alternative clinical markers?
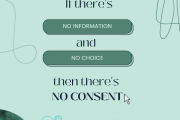
Informed consent is a critical principle in healthcare. A recent Australian survey revealed that many women lacked sufficient information and choice about fetal monitoring methods. Only 35% reported being asked for consent. This highlights a significant issue in maternity care, and it is well past time it was addressed.