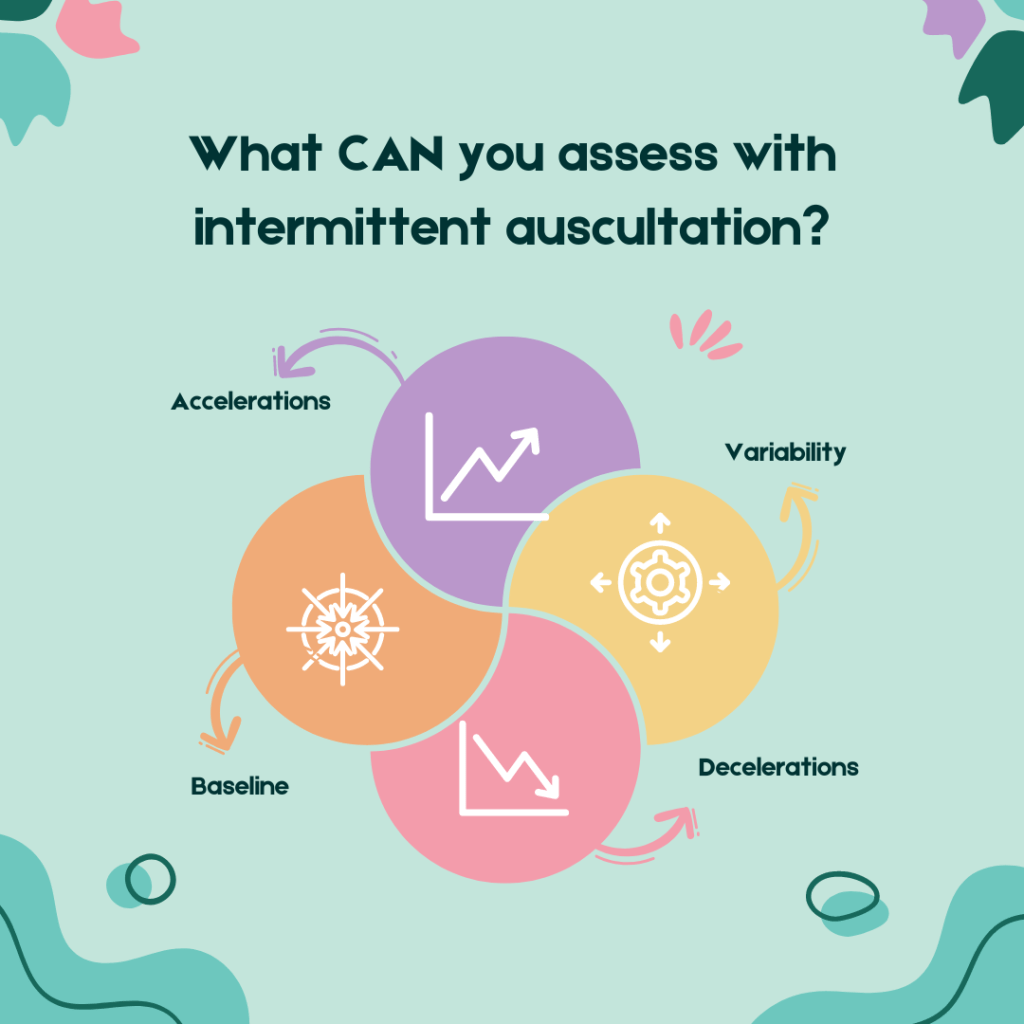
Let me begin, like the good researcher I am, by defining some terms. Intermittent auscultation is a type of fetal heart rate monitoring. A device of some sort is used to make it easy to hear the fetal heart rate, so the person listening (auscultating) can assess certain features of the heart rate, to determine whether it is considered normal or not. Typically, a handheld Doppler device is used. This is done intermittently, with one common approach being to listen for sixty seconds every 15 minutes during labour.
One of the features being assessed is the baseline. This is the average heart rate, measured in between contractions, when the fetus is at rest rather than moving, and not during a period where short term changes (accelerations or decelerations) are happening. Importantly, the baseline is not a flat line, with the amount of moment by moment wiggle up and down around the midpoint, called variability. None, too little, or too much, are considered to be signs that the fetus is responding to low oxygen levels, or some other external factor like the medications the woman has taken.
Fact or fiction: You can only determine variability with a CTG recording
As I read research and guidelines about fetal monitoring, I keep encountering authors who make the assertion that you can only measure variability by generating a CTG recording and looking at the graph. This “fact” is then sometimes used to argue that intermittent auscultation is inherently inferior to CTG monitoring as this is Really Useful Information TM. I think this is nonsense.
I’ll begin with a caveat – as an obstetrician, I was not the person spending hours doing intermittent auscultation during a woman’s labour. But it was my practice to always auscultate the fetal heart with a Doppler, with a screen displaying the heart rate when this technology became available, for at least a minute, during every antenatal visit other than in the first trimester. (It is too hard to find that early – so I would offer a scan instead.) So I do have first hand experience with the reality of what it is like to do intermittent auscultation, albeit not in labour.
And I certainly could tell when variability was normal, increased, or decreased. So when I hear people who are claiming to be experts say it can’t be done, I do wonder how they can’t possibly have the same experience I used to have with a Doppler in my hand. I think the origin of this fiction is historical. Let me explain.
Then and now: a brief history of fetal heart rate auscultation
The first device used to listen to the fetal heart rate was the precursor to the modern Pinard stethoscope. The sounds are quieter with a Pinard than with a Doppler. It requires concentration to count the individual heart beats over a period of time, to determine the heart rate. Some advise counting for a full sixty seconds, others counting for 15 seconds and multiplying by four, four times in the sixty second period. Counting to 147 in sixty seconds while looking at a second hand (or thereabouts – normal fetal heart rates are between 110 and 160, and can exceed 200 beats a minute sometimes) is pretty much the only thing you can do. No multitasking! While it might be possible to have a vague sense of how variable the heart rate is over time, I expect this would be impossible for most people to reliably detect most of the time.

Doppler technology made it much easier to hear the fetal heart rate. The same sort of technology built into CTG machines, that counted the sounds to determine the heart rate number, moment by moment, was later added. Many portable Dopplers now have a screen showing this number, saving you having to remember whether you were now up to 59. Or was it 69? Damn, I have to start again…
For anyone who has heard the fiction that the numbers on the screen are unreliable and you should still count while looking at a second hand – if this were true then ALL CTG machines using Doppler sensors would be wildly inaccurate. They aren’t, so neither is your hand held Doppler. You can trust what you see.
So how do you determine variability with a Doppler and a screen?
This is how I used to do it – if you have a different approach – please weigh in down in the comments box. I’m really keen to build my own knowledge on the different possibilities here.
Find the fetal heart sounds and look at the numbers on the screen while simultaneously listening. Establish that there is no contraction, and the woman doesn’t feel fetal movements right now. The numbers will bounce up and down as you watch and listen. Over ten seconds you might see 125 – 128 – 132 – 127 – 124 – 133 – 135 – 129 – 128 – 124 – 133 etc… Between 125 and 135 there is 10 beats of variability (this is considered normal), and it puts the middle of the range at 130 – which is the baseline. This is exactly the same thing people do when looking at the wiggly line on the CTG, but instead you are looking at the numbers instead. In the same way, you can also see / hear an acceleration or a deceleration.
So – to those people out there saying it can’t be done, I have some suggestion. First, stop saying it unless you have evidence to prove what you say is true. Then, stop and ask people what they are doing when they say they CAN determine variability with a Doppler during intermittent auscultation. And please, don’t conduct research based on the assumption it is impossible. This simply serves to reinforce the belief it is impossible when it isn’t!
Please – let me know your experiences! Can you tell variability when performing intermittent auscultation or not? What myths have you been told about it?
Sign Up for the BirthSmallTalk Newsletter and Stay Informed!
Want to stay up-to-date with the latest research and course offers? Our monthly newsletter is here to keep you in the loop.
By subscribing to the newsletter, you’ll gain exclusive access to:
- Exciting Announcements: Be the first to know about upcoming courses. Stay ahead of the curve and grab your spot before anyone else!
- Exclusive Offers and Discounts: As a valued subscriber, you’ll receive special discounts and offers on courses. Don’t miss the chance to save money while investing in your knowledge development.
Join the growing community of BirthSmallTalk folks by signing up for the newsletter today!
References
Categories: History, IA, Reflections
Tags: acceleration, baseline, Decelerations, Doppler, Pinard, variability
20 replies ›
Trackbacks
- How intermittent auscultation is done in the UK – Birth Small Talk
- Twenty fetal monitoring myths that won’t go away – Birth Small Talk
Hi,
Do you have any articles which lool at the evidence to show:
1) What you look for in variability represents fetal compromise, and
2) If variability looks good that this is reassuring?
Lay reader here, loving your work. Thank you.
Emma Ashworth
LikeLike
Thanks Emma
You’ll find definitions about “normal”, reduced, absent, and increased variability in fetal monitoring guidelines like the NICE guideline. https://www.nice.org.uk/guidance/ng229 These are based on opinion rather than sound evidence. People believe that normal patterns are reassuring of fetal wellbeing, and any of the abnormal patterns indicate low oxygen levels, but the evidence for this is a bit thin.
LikeLiked by 1 person
Agree! So refreshing to read your stuff. There is an unfortunate tendancy for senior midwives to fall in with ’emperor’s new clothes’ when a new edict or policy comes out and we are asked to throw away the evidence of ours eyes and ears over years of practice for a new slogan or new unevidenced practice. CTG is preferred over doppler because there is a paper or digital record for litigation purposes.
LikeLike
Ah yes – but who does that scrap of paper protect?
LikeLiked by 1 person
Kia ora 🙂
I am an LMC midiwfe from New Zealand, Aotearoa,
Wonderful to read this discussion as I do this for normal births.
In a similar method as you describe.
I listen with a visual display dopler for one minute throughout labour .
Approx every half hr in active first stage and then around every 10 mins
in second stage.. During the birth I ensure I listen at various points.
For example I may do a 1 minute auscilation between contractions and
when accessible during a mobile birth during a contraction and another
point during and after the contraction and similarly at the beginning
and during a contraction. I always record my readings as such. So I feel
I get a really good and clear assessment of foetal heart rates/patterns
throughout labour.
Examples of my documentation would be : Foetal heart rate for 1 min
during contraction (or after contraction or start of contraction – as
the case may be). I also record things like “no decels auscilated ” or
“good variability auscilated” or acels auscilated” for fullness of
recording and to try and satisfy doctors.
Still however I am told it is never as accurate as a ctg or some similar
comment.
As an aside. If I was to try and meet the local requirements of 5 min
auscilations in 2nd stage I would not be able to provide the midwifery
care and support to the woman in second stage. I find this protocol
nearly impossible to meet while supporting women to birth.
Glad you are bringing this up for discussion
Nga mihi
Fiona Heares
LikeLike
Thanks Fiona! What you are doing sounds great. There’s no research to tell us the ideal timing for when to listen. I think the key is to get to know the individual fetus and pay close attention to the events of labour. If anything feels a bit off, listen more frequently until you have it figured out.
LikeLike
In the home birth arena, IA with a Doppler is all we have (years ago I found Pinards or ear on the belly too hard in labour, and impossible in water birth, of course). So listening for 60 seconds is totally reassuring (or otherwise). It is perfectly possible to see, count and evaluate – even when the probe is under water. That (plus fetal movement, maternal position, liquor colour, maternal pulse, temperature etc) gives us plenty of information as to fetal wellbeing during labour and birth.
LikeLike
Thanks Alison – it is good to be reassured I was not imagining I was able to tell variability and that it is a common experience!
LikeLike
Hi Dr Small, I am a student midwife and I encourage my continuity women to read your blog or do your basics course. So far all of them have chosen intermittent auscultation over CTG which has meant bravely signing non-standard management plans and then letting ME auscultate because the hospital midwives are usually too busy (and frankly exasperated that this woman is doing something against guidelines) to do it. Works for me because as far as I’m concerned it’s great learning experience and it gives me something to do. At this point, I’m still learning and I don’t do it perfectly (but then, I don’t really know what “perfectly” is?). I listen roughly every 15 mins in first stage (but I think that is too much really) and a bit more frequently in 2nd stage (but many women like to decline me poking them and of course I respect that).
i like to listen through contractions and I feel ok if we return to baseline (which is of course a range, bouncing around, variability). But usually, I know what’s a normal average from reading the numbers and I document “140bpm” as the baseline – not a range as I might do antenatally. I don’t know why we do a range antenatally and a single number intrapartumly but that’s what I do. I’m not sure if I could tell if decels are late or not, I just know if it comes back. I also don’t especially LOOK for accelerations. Unless there is a way new baseline – suddenly tachy or Brady – I think we’re ok. However, as I recently witnessed a midwife shake her head and say “we don’t even have anymore accelerations” when a labour with an OP baby took a lull (babe possibly asleep), I’m wondering if I should be more concerned about accelerations to keep people happy that all is well?
love your work!
LikeLike
Hi Claire – it looks like I really need to get on and write a course about fetal physiology! You might want to read this paper – https://doi.org/10.1016/j.ejogrb.2022.04.021 It looks at the relationship between various heart rate patterns and neonatal encephalopathy. The presence of accelerations was more common with a healthy fetus, but not all healthy fetuses had accelerations, and some fetuses who developed encephalopathy had accelerations.
LikeLike
So, reading this paper, I feel like I have pretty much an equally as good a chance of NOT diagnosing a fetus with HIE as one with.
I am thinking about a Coroners report that we had to study for Uni that involved several midwives who failed to INSIST on a CTG on arrival to hospital and failed to adequately document auscultated FHR readings. It was determined that they were responsible for the intrauterine death of Samara because, had there been flags raised earlier, she could would have been born via c-section without injury.
Knowing what I (think) I know about FHR monitoring, I feel like they got a really bad rap. Is it fair for me to say – even if they had monitored to current day RANZCOG approved standards and had done everything by the book, that baby might well still have died? In which case, this feels like a horrible injustice for everyone involved AND, what are we teaching students by scaring the living daylights out of them with case studies like this one? We should not be telling parents we know things that we can’t know.
https://www.courts.qld.gov.au/__data/assets/pdf_file/0006/86577/cif-hoy-sl-20110405.pdf
LikeLike
The legal system perpetuates the myth that if only CTG monitoring had been used (rather than intermittent auscultation), the baby would be alive today. There is no evidence to back up that belief. There were other significant issues in this case (long periods with apparently no intermittent auscultation, no action taken when the baseline was rising, inadequate documentation followed by modifying the record, lack of good communication with the obstetrician.) What stands out for me the most is that no one involved in her care ever discussed the pros and cons of CTGs and intermittent auscultation with her or made space for the woman to decide what she wanted.
LikeLike
Hi Kirsten, congrats on your birthday!I would like to log on so I can more easily leave comments….but a colleague of mine several years ago logged on using my computer – we shared it for client notes etc- and I can only log on as Sharyn (talestotell) and I’d rather be me! I have midwifed clients who did not want any ultra sound to be used for them, antenatally and in labour. I have a wooden pinard, about 35 years old and am very used to using it. I can hear decelerations and accelerations, if the woman is still and not fat. I do find my doppler much easier and like that the sounds can be heard by all.As always I enjoy your posts.Chris Chris Warren Midwife York Storks Midwifery Support 01423360460
LikeLike
Kirsten,
Many years ago a US midwife named Lisa Paine published an article on doing IA using a fetoscope, in what was then called the Journal of Nurse-Midwifery, the official pub of the American College of Nurse-Midwives. When I have time, I will try to get it for you. She showed that you could assess variability and accels/decels with it.
I don’t know how familiar you are with fetoscopes – in Oz it’s all CTG, handheld Dopplers, or Pinards, and (as a musculoskeletal disorder researcher) I don’t like Pinards for the body position required. A fetoscope still requires bending, but not with the neck twist. Inexpensive to buy. Maybe we could get fetoscopes going in Oz together!
Hope you are well!
Cheers, Maryann
>
LikeLike
I’d love to read it, if you can locate it. And yes, let’s get fetoscopes going internationally!
LikeLike
Kirsten,
As promised: I didn’t find the article I was looking for, but I found this. It summarizes a study that compared outcomes after auscultated accels vs. NST, by Lisa Paine et al.
https://pure.johnshopkins.edu/en/publications/a-comparison-of-the-auscultated-acceleration-test-and-the-nonstre-3
And this is a later article on auscultated accels methods

Cheers, Maryann
>
LikeLike
I found it, and can see several other publications from her on Google Scholar. Thanks for introducing me to her work – I shall investigate further!
LikeLike
I am glad that I wasn’t the only one who felt that way. I always thought that doppler gives you good chunk of information, specially in underdeveloped countries where CTG is not widely available
LikeLiked by 1 person